Research
Study reveals new details about skeletal cell ageing
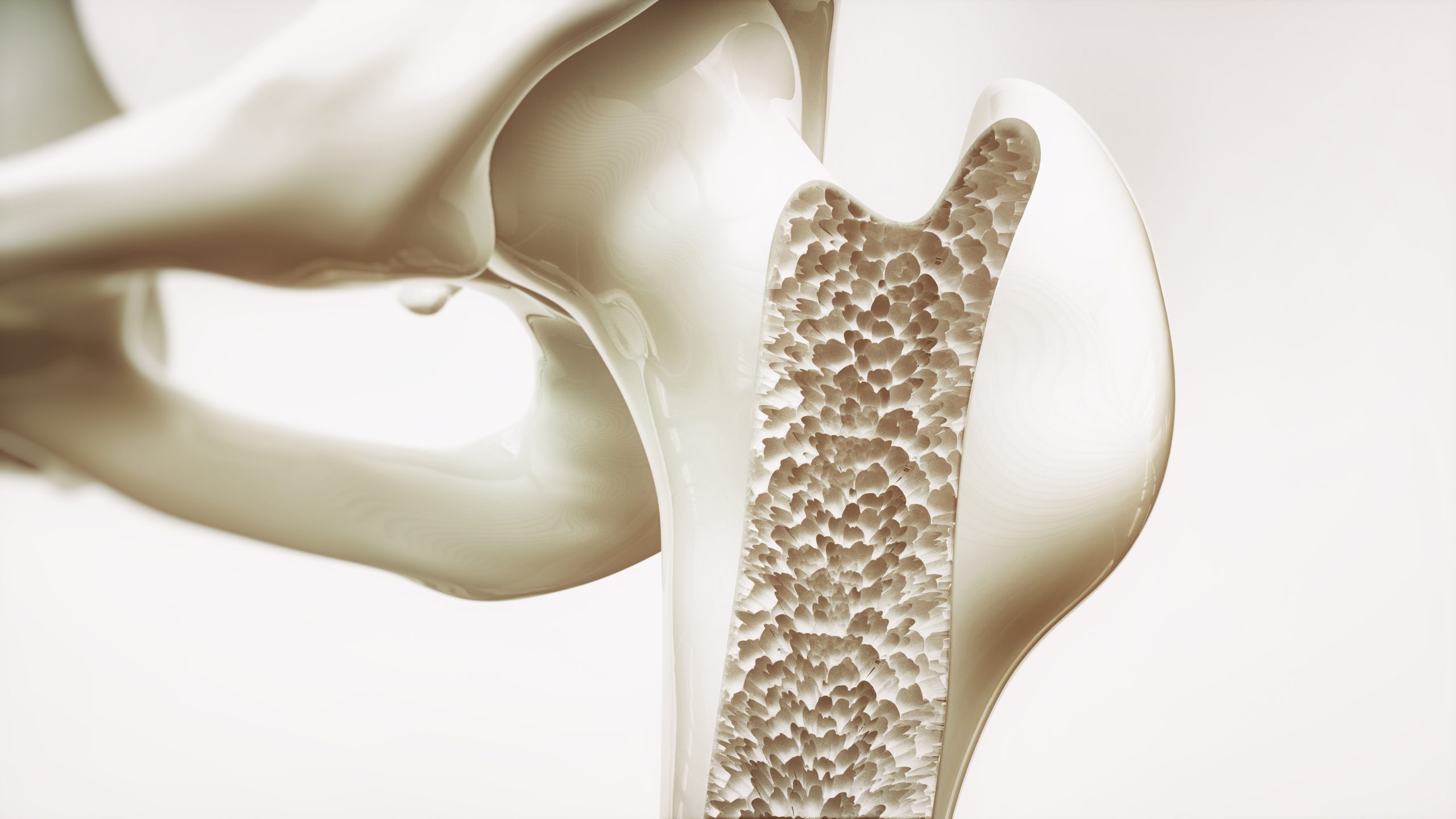
A new study has found that osteocytes – a type of bone cell – undergo dramatic structural and functional changes with age that impair their ability to keep our bones strong, offering new insights that could pave the way for better treatments for osteoporosis and age-related bone loss.
Ageing and stress can induce cellular senescence in osteocytes, resulting in cytoskeletal and mechanical changes that impair their ability to sense mechanical signals, ultimately weakening bone.
Osteocytes are the master regulators of bone health, sensing mechanical forces and directing when to build or break down bone. But when exposed to senescent cells – damaged cells that stop dividing but don’t die – osteocytes themselves begin to stiffen. This cytoskeletal stiffening and altered plasma membrane viscoelasticity undermine their ability to respond to mechanical signals, disrupting healthy bone remodelling and leading to bone fragility.
“Imagine the cytoskeleton as the scaffolding inside a building,” said Maryam Tilton, assistant professor in the Cockrell School of Engineering’s Walker Department of Mechanical Engineering and principal investigator of the study.
“When this scaffolding becomes rigid and less flexible, the building can’t adapt to changes and stresses, leading to structural problems. Similarly, stiffened osteocytes can’t effectively regulate bone remodelling, contributing to bone loss.”
Senescent cells release a toxic brew of molecules, called senescence-associated secretory phenotype (SASP), which triggers inflammation and damage in surrounding tissues. They’ve been linked to the development of cancer and many other chronic diseases. Until now, most research has focused on detecting senescence through genetic markers, a notoriously challenging task because these markers vary widely across cell types.
Tilton and her collaborators approach the issue from a different perspective, focusing on cell mechanics. Combining genetic and mechanical approaches could lead to improved treatments for ageing cells.
“Much like physical therapy helps restore movement when our joints stiffen, we’re exploring how mechanical cues might help reverse or even selectively clear these aging cells,” Tilton said.
“In the future, biomechanical markers could not only help identify senescent cells but also serve as precise targets for eliminating them, complementing or offering alternatives to current drug-based senolytic therapies,” added Dr. James Kirkland, principal investigator of the National Institutes of Health Translational Geroscience Network, director at the Center for Advanced Gerotherapeutics at Cedars-Sinai and a co-leader of the new research.
Improved knowledge about how bones age could improve treatments for osteoporosis. The condition leads to weakened bones and an increased risk of fractures and affects millions of people worldwide, particularly those over the age of 50. As the global population ages, understanding the mechanisms behind bone deterioration becomes increasingly important.
The team plans to expand their research by exploring the effects of different stressors on osteocytes and investigating potential therapeutic interventions.
Wellness
Roundup: Atlas maps molecular fingerprints of health, disease and ageing

Age Tech World explores the latest research developments in the world of ageing and longevity.
Pan-disease atlas maps molecular fingerprints of health, disease and ageing
A new study has mapped the distinct molecular “fingerprints” that 59 diseases leave in an individual’s blood protein, which would enable blood tests to discern troubling signs from those that are more common.
An international team of researchers mapped how thousands of proteins in human blood shift as a result of ageing and serious diseases, such as cancer and cardiovascular and autoimmune diseases.
The Human Disease Blood Atlas also reveals that each individual’s blood profile has a unique molecular fingerprint, which changes through childhood and stabilises in adulthood.
This provides a baseline for comparison that healthcare providers could one day use to flag early deviations.
The study used machine learning that enables information critical for building blood panels that would not misclassify patients in real world settings.
The mapping of molecular fingerprints of disease is a crucial step for building blood tests that work in the clinic, the researchers say.
For example, many proteins that rise in cancer or autoimmunity also rise in infections, reflecting shared inflammatory pathways, while other patterns such as liver-related conditions are clustered by organ systems.
The Disease Blood Atlas offers a path to solve the problem of identifying reliable, reproducible biomarkers for diseases – a process that to date has typically involved comparing new protein markers against a control, that is, a healthy profile.
The researchers point to the study’s success in identifying common biomarkers that are consistently altered in various conditions.
These shared molecular features could serve as universal diagnostic, prognostic or therapeutic targets.
Among the findings was that specific protein profiles can change substantially as individuals approach a cancer diagnosis, with some proteins showing higher concentrations prior to diagnosis.
These findings suggest more study should be devoted to investigating the potential of using proteomics for early cancer detection.
Aging Well with AI report explores AI and the healthcare workforce
The “Aging Well with AI: Empowering Care through Innovation” whitepaper has been published, the first in a two-part white paper series exploring how artificial intelligence (AI) can strengthen the U.S. healthcare workforce and improve access to care.
As the US confronts a historic shortage of healthcare workers alongside a rapidly ageing population, the report outlines specific ways AI can reduce strain on clinicians and improve outcomes for older adults, without eroding the human relationships that are essential to high‑quality medicine.
HealthFORCE, a national alliance of leaders dedicated to addressing the root causes of America’s healthcare workforce crisis, along with the American Academy of Physician Associates (AAPA) and West Health, published the report.
The paper highlights five opportunities for AI to extend the healthcare workforce and improve care for older adults and calls on policymakers, health systems and innovators to invest in geriatric-focused tech innovation and prioritise AI tools that serve older adults.
It also calls for incentives for cross-specialty training in ageing care and AI use for all frontline providers, the establishment of national standards for AI integration across state lines and care settings and the promotion of interoperability and support value-based payment models that reward continuity, efficiency, and prevention.
The upcoming second report will focus on how AI can augment care delivery across all patient populations and help address the projected shortfall of 3.2 million healthcare workers by 2026.
It is set to be released later this month.
Lifelong companionship protects ageing rat brains from cognitive decline
A new research paper shows that aged rats who lived in socially enriched environments throughout life retained better memory and cognitive flexibility than those housed alone.
This study highlights the importance of social interaction in protecting the ageing brain.
Cognitive decline, such as memory loss and reduced problem-solving ability, affects many people over the age of 65.
While many factors contribute to age-related cognitive decline, this study suggests that one key factor may be surprisingly simple: long-term social connection.
To explore how social interaction might influence memory performance and brain activity, the researchers designed a study using rats as a model for ageing in humans.
The team compared three groups of rats: young adults, aged rats housed alone, and aged rats housed socially in groups.
All groups had access to the same physical enrichment, such as exercise and stimulating objects, but only some experienced lifelong social companionship.
The team tested these animals on a complex memory challenge known as the biconditional association task, which requires animals to make context-based decisions, an ability that typically declines with age.
The results showed that aged rats living in social groups performed just as well as young adults on the memory task, while those housed alone showed significant impairments.
Socially housed rats also made fewer working memory errors and required less effort to complete cognitive tasks, suggesting not only better performance but more efficient brain function.
These benefits were not observed in aged rats who received only environmental enrichment without social interaction.
Brain imaging revealed additional differences between the groups.
Socially housed aged rats showed increased activity in the hippocampus, particularly in the CA3 region, which plays a key role in forming and separating memories.
In contrast, aged rats that lived alone had lower activity in this region, which may explain their poorer performance.
Interestingly, socially housed rats also showed reduced overactivity in the anterior cingulate cortex, a brain area involved in attention and decision-making, suggesting a more balanced and efficient neural response.
This research provides new insight into how lifelong social experiences shape brain health during ageing.
While earlier studies have shown that physical activity and cognitive stimulation help preserve cognitive function, this study identifies social interaction as an independent and powerful protective factor.
The findings are consistent with human studies showing that older adults who remain socially active tend to experience slower cognitive decline and stronger brain function.
Overall, these results emphasise that brain ageing is not inevitable but may be influenced by our social environments.
This research suggests that fostering lifelong social connections could be a critical, low-cost strategy to protect memory and mental flexibility in older adults.
Service dogs slow cellular ageing in female veterans
New research has found that service dogs may help slow biological ageing in women.
This groundbreaking study, focused on female veterans in the United States, is among the first to examine the impact of working with service dogs on this often-overlooked population.
By measuring biological indicators of stress, the researchers have uncovered a key insight: the way stress is felt emotionally doesn’t always reflect how it affects the body at a cellular level.
Researchers conducted the study involving female veterans with post-traumatic stress disorder (PTSD), but instead of receiving service dogs, these women volunteered to train them for fellow veterans in need, offering support not just to others, but potentially to themselves.
The study examined whether this purposeful, mission-driven activity could reduce both biological and psychological stress, and whether previous combat exposure influenced those effects.
Until now, the emotional and therapeutic benefits of such unique relationships have been largely unexamined in female veterans.
To measure biological stress, researchers looked at telomere length (a marker of cellular ageing) using saliva samples, and heart rate variability (HRV), a sign of nervous system balance, using wearable monitors in participants in the service dog training program group or a comparison group that watched dog training videos.
Psychological stress was assessed using validated questionnaires measuring PTSD symptoms, perceived stress, and anxiety at multiple points during the study.
Results evealed promising biological benefits associated with service dog training, particularly for veterans with combat experience, while improvements in psychological symptoms were seen across all participants, regardless of the intervention.
One of the most striking findings involved telomere length. Veterans who participated in the dog-training programme showed an increase in telomere length, suggesting a slowing of cellular ageing.
In contrast, those in the control group exhibited a decrease in telomere length, indicating accelerated ageing.
Combat experience significantly influenced these results: veterans with combat exposure who trained service dogs experienced the greatest gains in telomere length, whereas those with combat exposure in the control group saw the most pronounced declines.
On the psychological front, both groups, those who trained dogs and those in the control group, reported significant reductions in PTSD symptoms, anxiety and perceived stress over the eight-week period.
However, these mental health improvements were similar across groups, suggesting that simply participating in the study and receiving structured attention may have offered therapeutic value.
Unlike the biological findings, psychological outcomes did not appear to be affected by combat exposure.
The study also suggests that the skills learned during service dog training such as positive reinforcement and reading animal behavior may have strengthened participants’ bonds with their own pets at home, offering additional emotional support.
Unlike general volunteering, service dog training uniquely blends emotional healing with building a close relationship between veterans and their animals, providing therapeutic benefits that go beyond typical community engagement.
Female veterans aged 32 to 72 were randomly assigned to either the service dog training program group or a comparison group that watched dog training videos.
Both groups took part in one-hour sessions each week for eight weeks. Researchers measured outcomes before, during and after the programme.
These findings provide early evidence that non-pharmacological interventions – such as service dog training – may help reduce the physical toll of stress and slow cellular ageing in female veterans.
News
Cholesterol-lowering drugs could reduce dementia risk

People with genetic variants that naturally lower cholesterol were found to have up to 80 per cent lower dementia risk in a study of more than one million participants.
The research analysed data from Denmark, England and Finland to assess how genes that mimic the effects of cholesterol-lowering drugs such as statins and ezetimibe influence dementia risk.
Scientists found that reducing blood cholesterol by one millimole per litre was linked to as much as an 80 per cent reduction in dementia risk for certain drug targets, suggesting possible benefits from cholesterol-lowering treatment.
The researchers used a method known as Mendelian randomisation, which allows scientists to study the effects of lowering cholesterol while avoiding confounding factors such as diet, weight and other lifestyle habits.
Dr Liv Tybjærg Nordestgaard led the research while at Bristol and now works at Copenhagen University Hospital–Bispebjerg and Frederiksberg hospital.
Dr Nordestgaard said: “What our study indicates is that if you have these variants that lower your cholesterol, it looks like you have a significantly lower risk of developing dementia.”
Some people are born with genetic variants that naturally affect the same proteins targeted by cholesterol-lowering drugs such as statins and ezetimibe.
By comparing these individuals with those without such variants, the researchers were able to measure differences in dementia risk.
Mendelian randomisation uses genetic variation as a natural experiment.
Because genes are inherited randomly at conception, this method can mimic randomised clinical trials and offer stronger evidence for cause-and-effect relationships than traditional observational research.
The findings suggest that having low cholesterol, whether due to genetics or medical treatment, could help reduce the risk of developing dementia. However, the study does not provide definitive evidence about the effects of the medicines themselves.
One of the main challenges in dementia research is that symptoms typically appear later in life, requiring decades of follow-up to detect meaningful changes. This makes long-term clinical trials difficult to conduct.
The biological link between high cholesterol and dementia is not yet fully understood. Dr Nordestgaard suggested that atherosclerosis — the build-up of cholesterol in blood vessels — may play a key role.
Dr Nordestgaard said: “Atherosclerosis is a result of the accumulation of cholesterol in your blood vessels.
“It can be in both the body and the brain and increases the risk of forming small blood clots—one of the causes of dementia.”
Blood clots can block small vessels in the brain, leading to vascular dementia — the second most common form of the condition after Alzheimer’s disease.
Even small clots can damage brain tissue over time and contribute to cognitive decline.
The study used data from large genetic research projects including the UK Biobank, the Copenhagen General Population Study, the Copenhagen City Heart Study, the FinnGen study and the Global Lipids Genetics Consortium.
These resources provide genetic and health information from diverse populations, improving the reliability of the findings across different ethnic and geographical groups.
The UK Biobank includes data from around 500,000 participants aged 40–69, while the Copenhagen studies have tracked Danish populations for several decades, providing detailed health records for long-term analysis.
“It would be a really good next step to carry out randomised clinical trials over 10 or 30 years, for example, where you give the participants cholesterol-lowering medication and then look at the risk of developing dementia,” Dr Nordestgaard added.
Such trials would provide direct evidence about whether cholesterol-lowering drugs can prevent dementia, rather than relying on genetic data.
However, their length and cost make them difficult to conduct.
Markets & Industry
New drug enhances GLP-1 weight loss without extra added effects, trial finds

Nimacimab significantly enhanced weight loss when combined with GLP-1 therapy without adding side effects, according to mid-stage clinical trial results involving 136 adults.
The experimental drug targets the body’s endocannabinoid system differently from existing weight-loss medications, offering a potential new approach to treating obesity when used alongside drugs such as semaglutide.
Participants given both drugs lost an average of 13.2 per cent of their body weight over 26 weeks, compared with 10.25 per cent for those on semaglutide alone — a statistically significant difference of nearly 3 per cent.
Skye Bioscience’s CBeyond study tested the first-in-class monoclonal antibody, which blocks CB1 receptors involved in appetite regulation and fat storage. The CB1 receptor is part of the endocannabinoid system, which helps control hunger, metabolism and fat accumulation. When these receptors become overactive, they can promote weight gain.
“This is the first clinical study to show that the combination of a CB1 inhibitor and a GLP-1 therapeutic can drive clinically meaningful additional weight loss beyond a GLP-1 drug alone,” said Louis Aronne, past president of The Obesity Society and clinical adviser to Skye Bioscience, the drug’s developers.
“Equally important, although the sample size is small, nimacimab achieved this without neuropsychiatric or additive gastrointestinal adverse events. I believe these results warrant further evaluation of the therapeutic potential of this novel CB1 inhibitor.”
Previous CB1-blocking drugs were abandoned because of psychiatric side effects such as anxiety and depression. Nimacimab has been engineered to stay outside the brain, potentially avoiding the problems that affected earlier drugs targeting this pathway.
In the 26-week trial, adults with overweight or obesity were randomly assigned weekly injections of nimacimab, semaglutide (the active ingredient in Wegovy), both drugs together, or placebo.
When used alone, nimacimab produced modest results — participants lost 1.5 per cent of their body weight compared with 0.26 per cent for placebo, a difference that was not statistically significant. Researchers said exposure to the 200 mg dose was lower than expected, suggesting higher doses may prove more effective.
“The 200 mg monotherapy arm provided important pharmacokinetic insight, showing that lower-than-expected drug exposure may have limited the observed effect and informing the dose-ranging strategy we are developing,” said Puneet Arora, the company’s chief medical officer.
Pharmacokinetic data describe how the body absorbs, distributes, metabolises and eliminates a drug, helping determine optimal dosing.
“At the same time, the combination of nimacimab with semaglutide produced a clinically meaningful additional weight loss that exceeded semaglutide alone, with a favourable tolerability profile even in patients who achieved the highest exposure levels.”
The most striking results came from the combination therapy. All participants receiving both drugs lost more than 5 per cent of their body weight, compared with 85 per cent of those on semaglutide alone. Two-thirds of the combination group lost more than 10 per cent, versus 50 per cent with semaglutide alone.
Importantly, the combination produced a healthier lean-to-fat mass ratio, indicating weight loss came primarily from fat reduction rather than muscle loss — addressing a concern that some GLP-1 drugs may cause skeletal muscle wastage.
Weight loss was still ongoing at the end of the 26-week study, suggesting further reductions could occur with longer treatment.
Safety findings were encouraging across all treatment groups. No neuropsychiatric side effects — such as anxiety, depression or insomnia — were reported with nimacimab, either alone or combined with semaglutide.
Gastrointestinal side effects, a leading cause of discontinuation with GLP-1 therapies, did not increase when nimacimab was added to semaglutide. These typically include nausea, vomiting, diarrhoea and constipation.
The overall discontinuation rate was 27 per cent, with only 3.7 per cent of participants dropping out due to adverse events — most of them in the placebo group.
“Gastrointestinal side effects remain a leading cause of discontinuation with obesity therapies,” said Sean Wharton, director of the Wharton Medical Clinic and a clinical adviser to Skye Bioscience.
“It was notable that nimacimab did not increase GI adverse events while adding clinically meaningful weight loss in combination with semaglutide. In my view, a next study with higher nimacimab dosing is the logical step to fully define its role in clinical practice.”
“With our preclinical data, toxicology safety margin, and PK modelling, we believe we have a path to support higher dosing, and we are evaluating the next stage of development to optimise dosing in potential future clinical trials,” Arora said.
Participants from the Phase 2a study are continuing in a 26-week extension trial, with results expected in early 2026. This will provide data on the longer-term efficacy and safety of the combination approach.
GLP-1 drugs such as semaglutide mimic a hormone that regulates appetite and blood sugar. While highly effective for weight loss, some studies have raised concerns about side effects including kidney injury, skeletal muscle loss and gastrointestinal issues.
A combination therapy that enhances weight loss without compounding side effects could address a major unmet need in obesity treatment, where many patients struggle with the tolerability of current medications.

 Wellness2 months ago
Wellness2 months agoMillions with type 2 diabetes should get personalised care and new medicines, says review

 News1 month ago
News1 month agoRound up: First AI-powered app for longevity and more

 Insights1 day ago
Insights1 day agoHigh fat diet may keep brain young, study suggests

 News2 months ago
News2 months agoBetter nutrition and tailored exercise programmes key to preventing care home falls

 Insights3 weeks ago
Insights3 weeks agoNHS warns against dismissing symptoms as ‘natural part of ageing’

 Insights1 month ago
Insights1 month agoAir pollution can drive devastating forms of dementia, study suggests

 News2 weeks ago
News2 weeks agoWeight loss jabs should be first-line obesity treatment in most cases, new guidance states

 News2 months ago
News2 months agoGetting a hearing aid before 70 may sharply cut dementia risk, study shows




































