Wellness
Study aims to improve recovery after cancer treatment in older people

Researchers are studying recovery after bowel cancer treatment in older people, as the REBOUND study looks at ageing changes linked to surgery and care.
The study, Resilience Breakthroughs in Older people Undergoing cancer proceDures, is examining how key “hallmarks of ageing” are affected following bowel cancer treatment in people aged 65 and over.
These are the biological processes that naturally occur as we get older.
The chief investigator and principal investigator of the study, professor Thomas Jackson is professor in geriatric medicine at the University of Birmingham and consultant in geriatric medicine and general internal medicine at University Hospitals Birmingham (UHB).
He said: “This is really important work that couldn’t be done without the support of patients agreeing to be in the study.
“We want to understand how the biology of ageing changes when older people have significant events, such as major surgery, and why some people recover well, and others don’t.
“With this understanding, we can identify ways of improving recovery in everyone and maximising the benefits of cancer treatment.”
Researchers at USB, in collaboration with King’s College London (KCL), are leading the study to understand the factors that influence how well older people recover from cancer treatment and to find ways to keep the body strong.
While age is a known risk factor for developing cancer, treatments such as chemotherapy, immunotherapy (which helps the immune system attack cancer), surgery and radiation therapy can trigger processes in the body that resemble ageing.
By understanding how the body responds to cancer treatment, researchers aim to develop new interventions that could prevent or reduce ageing-related changes and improve the number of years spent in good health. The ultimate goal is to help older people with cancer remain active and continue doing the things that matter most to them.
The study involves analysing DNA for age-related changes, examining gut bacteria from stool samples and assessing changes in blood and fat cells.
Samples will be collected at multiple time points before, during and after surgery.
These biological findings will be compared with tests of memory, thinking, strength and muscle function, alongside information from medical records.
The study aims to recruit 172 participants aged 50 years and older who are scheduled to undergo bowel cancer surgery at UHB, Guy’s and St Thomas’ NHS Foundation Trust and King’s College Hospital NHS Foundation Trust.
The study opened to recruitment in autumn 2024, and to date, 58 patients have been enrolled.
The project is a collaborative effort bringing together clinicians specialising in the care of older people, surgeons and scientists with expertise in ageing and complex data analysis. It is supported by the Dynamic Resilience programme, funded by Wellcome Leap and the Temasek Trust.
News
Return to traditional lentil and rice diet could help curb diabetes in Nepal

Traditional dal bhat could help curb Nepal’s diabetes crisis, with one in five people over 40 living with type 2 diabetes, researchers say.
With medication often unaffordable, researchers are testing whether cheap, local staples such as lentils and rice can help tackle type 2 diabetes, where blood sugar stays high because the body does not make enough insulin or cannot use it properly.
If poorly controlled, type 2 diabetes can lead to complications including kidney disease, limb loss, blindness and premature death.
Dr Ashish Tamang, a resident doctor based in Kathmandu said: “For many families, diabetes is not just a medical condition, but a long-term social and economic burden.”
A pilot study in Kathmandu involving 70 hospital patients with long-established diabetes put 43 per cent into remission after a calorie-controlled traditional diet.
An ongoing trial involving 120 people in villages and communities on the outskirts of cities has shown similar promise.
“It is very early days but around half are free from diabetes at four months, with an average weight loss of only 4 to 5kg,” said Prof Mike Lean, a diabetes and human nutrition expert from the University of Glasgow.
The work is being expanded in a four-year study led by the University of Glasgow in collaboration with Dhulikhel hospital in Nepal, which also aims to test whether the diet can prevent type 2 diabetes in people at high risk.
The approach builds on work by a UK team, including Lean, who showed in 2017 that weight-loss diets based on soups and shakes could reverse type 2 diabetes. That programme is now part of standard NHS diabetes care.
People from Asian backgrounds are genetically predisposed to type 2 diabetes, meaning they can develop the condition after gaining relatively small amounts of weight. But the same pattern means less weight loss may be needed to reverse it.
Lean said the weight loss needed in Nepal is around half that typically required in the UK, where patients often need to lose 10 to 15kg. ‘It makes the task a fair bit easier,’ he said.
Participants were asked to follow an 850-calorie-a-day plan for eight weeks, typically with yoghurt and fruit for breakfast and main meals of lentils and rice, known as dal bhat.
They then moved to a higher-calorie version of the same diet to help maintain the lower weight.
During screening camps, people found to have diabetes, or to be at high risk, were given a cup, measuring glass and weighing equipment alongside a diet plan to help them stick to portion sizes.
They were also invited to attend regular support group sessions.
The programme was designed to be delivered in communities without the need for doctors or hospitals, supported by the female volunteers who underpin Nepal’s health system.
Trial documents describe a plan that ‘stresses a disciplined (traditional) eating pattern, avoiding snacking and high-fat/sugar processed western-type foods’.
A 2025 study found 87 per cent of packaged foods sold in Kathmandu shops exceeded World Health Organization recommended thresholds for sugar, fat and salt.
Lean said the approach was ‘not rocket science’. But it was ‘way more effective than any drug or medicine, and traditional medicines that don’t do anything’.
He also encouraged participants to switch to brown rice rather than double-milled white rice, which contains fewer nutrients, including lower levels of vitamin B1, which helps the body process carbohydrates.
The expanded study initially won UK government funding but was affected by cuts.
The Howard Foundation has stepped in with £1.78m to keep it going, and the project will also create educational materials on the drivers of diabetes.
Lean blames soaring type 2 diabetes rates in Nepal on the importation of western junk foods.
He said he had spoken to Nepalis who ‘remember the first bicycle arriving in their village’, adding that the bike was carrying sweets and soft drinks, and that improved transport links later brought more junk food.
Lower activity levels linked to technology are also a driver, the study team said.
Lean said officials from neighbouring countries have expressed interest at conferences. ‘If this works in Nepal, it will work for us,’ he said they told him.
News
Cognition and Cera expand Alzheimer’s clinical trials access

Cognition Health and Cera have partnered to expand access to Alzheimer’s clinical trials across the UK.
The collaboration links Re:Cognition Health’s specialist brain health clinics and trial expertise with Cera’s 2.5 million monthly home care visits, creating new pathways to identify and support people earlier in their health journey.
By connecting home care with specialist research centres, the partners aim to offer more people the chance to join studies, giving access to advanced assessment and emerging treatments while contributing to future therapies.
Dr Ben Maruthappu MBE, chief executive and founder of Cera, said: “Many older adults are currently ‘invisible’ to the clinical trials research system because they cannot access traditional clinic-centric recruitment.
“By enabling responsible, consented identification and screening within the home, we can bridge the gap between the community and the clinic.
“We are offering the older generation a seat at the table of global drug discovery, ensuring that the path to a cure starts where they are most comfortable—in their own daily lives.”
Re:Cognition Health has contributed to the development of lecanemab (Leqembi) and donanemab (Kisunla) through international trials, introducing disease-modifying approaches that are reshaping early intervention in Alzheimer’s care.
Older adults remain under-represented in research. NIHR data indicate only about 15 per cent of trial participants are 75 or older, despite high multimorbidity in this group. Dementia trial recruitment in the UK also lags other disease areas.
Through this collaboration, individuals who have not yet accessed specialist memory services can be referred earlier for assessment and potential study participation, with access to new-generation therapies where appropriate.
Cera’s technology-enabled home healthcare model, with daily patient contact and consented data capture, allows timely referral of potential participants from familiar settings to Re:Cognition Health clinics.
Together, the organisations will support earlier and more equitable participation by leveraging Cera’s scale and real-time insights. Carers and nurses deliver visits roughly every second on average, enabling early identification of those who may benefit from memory assessment.
Dr Emer MacSweeney, chief executive and founder of Re:Cognition Health, said: “With one in three people expected to develop dementia in their lifetime, it is essential that we create more inclusive and accessible routes into research.
“This collaboration enables us to extend our reach beyond traditional clinic settings and ensure that people who may benefit from early assessment and research participation are supported to do so.
“Clinical trials offer individuals access to the most advanced diagnostics and emerging treatments, alongside expert medical oversight.
“By identifying people earlier and guiding them through every stage of their journey, we can help improve participants’ experience and potential outcomes, while accelerating the development of the next generation of Alzheimer’s therapies.”
Wellness
Interview: Dr Matthew Bennett on building resilience and a pain-free healthspan
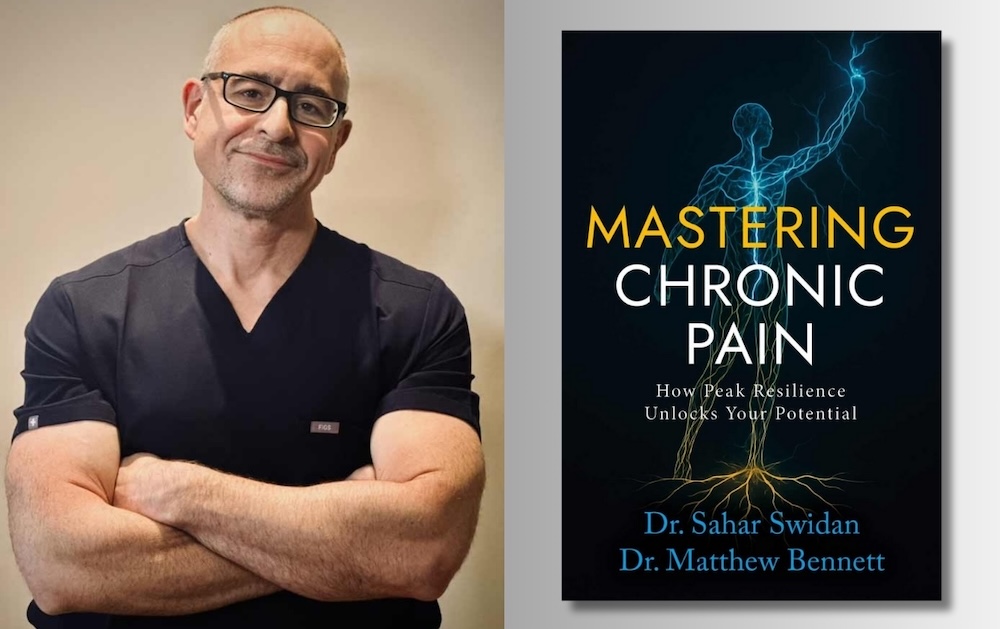
Harnessing the multi-dimensional capabilities of the human body is key to overcoming chronic pain and boosting longevity, say the authors of a new book.
While the primary focus of established health care systems is to target pain points through medication or surgery a more holistic approach is emerging, as US chronic pain doctor Matthew Bennett explains.
Published late last year by Dr Bennett and colleague Dr Sahar Swidan’s book, Mastering Chronic Pain: How Peak Resilience Unlocks Your Potential offers grounded insights into pain resolution.
Speaking to Agetech World from his New York base he said: “I’ve been treating patients in chronic pain for over 20 years.
“And, it becomes obvious that while some pain is very responsive to simple interventions, like a nerve block or a surgery, there’s a large number of people which that does not move the needle for.
“We used to look at it like, ‘Hey, the MRI shows this one spot that’s pushing on this one nerve. If we can take that spot off that nerve, everything’s going to be better’.
“And, that just doesn’t always play out that way. It’s become apparent that there are a lot of situations where the problem is more systemic.
“It’s really more of a metabolic problem, and pain is the expression of these system failures.”
‘Fight or flight’
The upstream drivers of acute pain can be numerous as Dr Bennett explains: “You can take as much pressure as you want off of nerves, but if your inflammatory system isn’t fixed, if the neurological system isn’t fixed, if your autonomic nervous system – meaning your fight-or-flight versus your rest-and-relaxation – isn’t balanced, if your gut biome is off, if your sleep is off – a lot of these problems aren’t going to improve.”
Key elements in developing a longevity-focused healthpsan – devoid of chronic pain and opioids – are simple, every day measures, focused on movement, sleep and breathing.
This includes developing the right muscles to create a ‘good deep core musculature’.
He continued: “An even bigger one is the way people breathe – the way they use their diaphragm.
“The diaphragm is a great big muscle that controls the deep core part of the spine. When the diaphragm’s not working correctly, the whole core musculature isn’t working right.
“You can’t get that stability in the lower spine, so other muscles jump in and try to do the work for you. That causes downstream problems.
“You need someone getting to that root cause,.. (and) we teach people how to do that, and they’ll have big breakthroughs.”
He continued: “Sleep is a big problem in people with chronic pain. There’s a lot of healing that occurs with deep sleep.
“Unfortunately, in a lot of pain states, sleep gets disrupted, and people can’t get into deep sleep, so the brain can’t clear itself of the byproducts of metabolism; that glymphatic system doesn’t work.
“Poor sleep also interferes with endocrine connectors; growth or sex hormones can be depleted. Obstructive sleep apnea can play a huge role. There’s just a big correlation between sleep disorders and chronic pain.”
Seeking calm
These key elements of Dr Bennett’s work – which has been described as ‘biopsychosocial’ – come concomitant with a keen focus on nervous systems, chronic inflammation and neuroplasticity.
Dr Bennett, co-founder of NoceViva, continued: “When we think about neurologics, one of the things that’s very far upstream of a lot of health is the balance between the fight-or-flight system and the rest-and-relaxation system – that autonomic nervous system.
“All of these things are ‘two-way streets’ with pain; meaning the pain can cause the dysfunction, and the dysfunction can cause the pain; it becomes this feedback cycle where things get entrenched in a bad loop.
“So, balancing that autonomic nervous system is a really helpful upstream fix to make. Simple things like breathwork. Some people do well with meditation.
“Some people do well with making sure they’re involved in hobbies. These are things that can help just calm that fight-or-flight system down.”
Nerves & neuroplasticity
Allowing ourselves to adjust to emerging health challenges is achievable in the right settings and with the right approach.
He continued: “The body’s nervous system has the ability to change. And it can change based on various inputs.
“The nervous system can become increasingly sensitised, or it can become de-sensitised. And so that’s one of the bigger things that we see in the chronic pain state, is this sensitisation that comes along with it.
“This neuroplasticity can make the nerves in the extremities more sensitive.
“It can also make the nerves in the central nervous system more sensitive – so nerves in the spinal cord, or even nerves in the brain can become hyper-sensitised – so they’re triggering more of a pain response in the person.
“But the same thing that can cause the system to go in what we would consider a bad direction, where it gets more sensitive, the neuroplasticity can actually become undone, and you can make the nerves less sensitive.”
AI to boost lifespan?
Looking ahead Dr Bennett foresees a future where a deeper understanding of the functional pathways of pain, combined with AI, stem cell therapies and regenerative biologics will all speak to a future of greater longevity for mankind.
“I think the more attentive we are to the root cause, the more attentive we are to functional pathways – when we start thinking about how the system really works? And we get out of just an algorithmic approach to things.
“We still have quite a ways to go. I think we are making progress. There was a time where we would not be thinking about any of this.
“I think everyone’s excited about what AI will bring. And are we going to be able to make some big steps? I think we’re able to intervene on a genetic level at this point.
“Will we be able to do it well enough to change lifespan? I would guess, yes, but by how much? I don’t know!”

 News4 weeks ago
News4 weeks agoNanoparticles target disease proteins in dementia

 Technology4 weeks ago
Technology4 weeks agoL-Nutra raises US$36.5m in series D funding

 Insights3 weeks ago
Insights3 weeks agoInterview: Dr Annu Navani on biotechnology and ‘the power to recode life itself’

 News4 weeks ago
News4 weeks agoGap partners with Spear Bio on Bio-Hermes-002

 Insights3 weeks ago
Insights3 weeks agoDentordu: Digital dentistry for healthier ageing

 News4 weeks ago
News4 weeks agoBioAge expands drug into diabetic macular oedema

 News3 weeks ago
News3 weeks agoStudy shows clear link between CTE and dementia risk

 Research4 weeks ago
Research4 weeks agoUSC funds AI projects for Alzheimer’s trials






























