Insights
Most liver cancer could be prevented through lifestyle changes and vaccination – study

Three in five liver cancer cases could be avoided through better hepatitis vaccination, reduced alcohol intake and efforts to tackle obesity, new research has found.
Without intervention, deaths from liver cancer are projected to rise from 760,000 in 2022 to 1.37m by 2050. The findings suggest 9m to 17m cases and 8m to 15m deaths could be prevented with targeted action.
The Lancet Commission on liver cancer found that reducing alcohol consumption, viral hepatitis B and C infections, and fatty liver disease could stop the majority of future cases.
Fatty liver disease occurs when excess fat builds up in the liver, which can lead to inflammation, liver damage and cancer.
Prof Jian Zhou of Fudan University in China, who led the research, said: “Liver cancer is a growing health issue around the world. It is one of the most challenging cancers to treat, with five-year survival rates ranging from approximately 5 per cent to 30 per cent.
“We risk seeing close to a doubling of cases and deaths from liver cancer over the next quarter of a century without urgent action to reverse this trend.”
Liver cancer is the sixth most common cancer worldwide and the third leading cause of cancer death.
The number of new cases is expected to nearly double from 870,000 in 2022 to 1.52m in 2050, largely due to population growth and ageing, with the steepest increases expected in Africa.
More than 40 per cent of global cases currently occur in China, which has high rates of hepatitis B infection.
One of the fastest growing causes is fatty liver disease, now referred to as metabolic dysfunction-associated steatotic liver disease (MASLD), which is linked to obesity.
About one-third of the global population is thought to have MASLD, which may be prevented by eating a balanced diet, staying active and maintaining a healthy weight.
Only 20 to 30 per cent of people with MASLD go on to develop the more severe form, metabolic dysfunction-associated steatohepatitis (MASH), which can lead to liver cancer.
The commission said MASH-linked cases are projected to increase from 8 per cent of liver cancer cases in 2022 to 11 per cent in 2050.
Alcohol is the second fastest growing cause, with alcohol-related liver cancer cases expected to rise from 19 per cent to 21 per cent by 2050
In contrast, hepatitis B-related cases are projected to fall from 39 per cent to 37 per cent, while hepatitis C-related cases are expected to decline from 29 per cent to 26 per cent.
Prof Hashem B El-Serag of Baylor College of Medicine in the US said: “Liver cancer was once thought to occur mainly in patients with viral hepatitis or alcohol-related liver disease.
“However, today, rising rates of obesity are an increasing risk factor for liver cancer, primarily due to the increase in cases of excess fat around the liver.”
The commission recommended that governments expand HBV vaccination, implement universal screening for adults, introduce minimum alcohol pricing and sugar taxes, add warning labels to unhealthy products, invest in early detection of liver damage and cancer, and improve palliative care services.
Dr Matt Hoare, associate professor in hepatology at the University of Cambridge’s Early Cancer Institute, said liver cancer was “unlike many other cancers” in that its death rate is still rising.
He noted that causes vary by region, and said Japan had successfully reduced its death rate by introducing preventive measures and improving early detection.
His team is now working to identify which liver disease patients are most likely to develop cancer using DNA sequencing of the liver.
News
Four in ten cancer cases could be prevented globally, report finds

Up to four in ten cancer cases worldwide could be prevented, a new global analysis has found.
The study examines 30 preventable causes, including tobacco, alcohol, high body mass index, physical inactivity, air pollution, ultraviolet radiation and, for the first time, nine infections that can cause the disease.
Released ahead of World Cancer Day on 4 February, the analysis from the World Health Organization (WHO) and its International Agency for Research on Cancer (IARC) estimates that 37 per cent of all new cancer cases in 2022, around 7.1 million cases, were linked to preventable causes.
Drawing on data from 185 countries and 36 cancer types, the study identifies tobacco as the leading preventable cause of cancer, globally responsible for 15 per cent of all new cancer cases, followed by infections (10 per cent) and alcohol consumption (3 per cent).
Three cancer types, lung, stomach and cervical cancer, accounted for nearly half of all preventable cancer cases in both men and women globally.
Lung cancer was primarily linked to smoking and air pollution, stomach cancer was largely attributable to Helicobacter pylori infection (a bacterial infection of the stomach lining), and cervical cancer was overwhelmingly caused by human papillomavirus (HPV).
Dr André Ilbawi, team lead for cancer control at WHO and author of the study, said: “This is the first global analysis to show how much cancer risk comes from causes we can prevent.
“By examining patterns across countries and population groups, we can provide governments and individuals with more specific information to help prevent many cancer cases before they start.”
The burden of preventable cancer was substantially higher in men than in women, with 45 per cent of new cancer cases in men compared with 30 per cent in women.
In men, smoking accounted for an estimated 23 per cent of all new cancer cases, followed by infections at 9 per cent and alcohol at 4 per cent.
Among women globally, infections accounted for 11 per cent of all new cancer cases, followed by smoking at 6 per cent and high body mass index at 3 per cent.
Dr Isabelle Soerjomataram, deputy head of the IARC Cancer Surveillance Unit and senior author of the study, said: “This landmark study is a comprehensive assessment of preventable cancer worldwide, incorporating for the first time infectious causes of cancer alongside behavioural, environmental and occupational risks.
“Addressing these preventable causes represents one of the most powerful opportunities to reduce the global cancer burden.”
Preventable cancer varied widely between regions.
Among women, preventable cancers ranged from 24 per cent in North Africa and West Asia to 38 per cent in sub-Saharan Africa.
Among men, the highest burden was observed in East Asia at 57 per cent, and the lowest in Latin America and the Caribbean at 28 per cent.
These differences reflect varying exposure to behavioural, environmental, occupational and infectious risk factors, as well as differences in socioeconomic development, national prevention policies and health system capacity.
Research
New study links Alzheimer’s memory loss to disrupted brain “replay” during rest
Memory problems in Alzheimer’s may be linked to disrupted brain replay during rest, new research suggests.
The study, conducted in mice, points to a disrupted brain process that normally helps strengthen and preserve memories.
Researchers say the findings could inform future drugs that target this malfunctioning process and guide tools for earlier detection.
Scientists at University College London (UCL) found that replay events occurred as often in mice with amyloid plaques (protein deposits linked to Alzheimer’s) as in healthy mice, but the underlying patterns were no longer organised.
Instead of reinforcing memories, the coordinated activity of place cells became scrambled.
Dr Sarah Shipley, co-lead author from UCL Cell and Developmental Biology, said: “Alzheimer’s disease is caused by the build-up of harmful proteins and plaques in the brain, leading to symptoms such as memory loss and impaired navigation, but it’s not well understood exactly how these plaques disrupt normal brain processes.
“We wanted to understand how the function of brain cells changes as the disease develops, to identify what’s driving these symptoms.
“When we rest, our brains normally replay recent experiences, this is thought to be key to how memories are formed and maintained.
“We found this replay process is disrupted in mice engineered to develop the amyloid plaques characteristic of Alzheimer’s, and this disruption is associated with how badly animals perform on memory tasks.”
This replay activity takes place in the hippocampus, a region essential for learning and memory. During rest, specific neurons known as place cells activate in rapid sequences that mirror recent experiences.
Place cells, discovered by Nobel Prize-winning UCL neuroscientist Professor John O’Keefe, are neurons that correspond to particular locations.
As a person or animal moves through a space, different place cells fire in sequence. Later, during rest, those same cells typically reactivate in the same order, helping the brain store the experience as a memory.
To study this process, researchers tested how mice performed in a simple maze while recording brain activity at the same time.
Using specialised electrodes, they monitored roughly 100 individual place cells simultaneously as the animals explored and then rested.
This approach allowed the team to compare normal replay patterns with those seen in mice that had developed amyloid pathology associated with Alzheimer’s disease.
The researchers also observed that place cells in affected mice grew less stable over time. Individual neurons stopped reliably representing the same locations, especially after rest periods, which are normally when replay should strengthen memory signals.
These changes had clear behavioural effects.
Mice with disrupted replay performed worse in the maze, frequently revisiting paths they had already explored and appearing unable to remember where they had been.
Professor Caswell Barry, co-lead author from UCL Cell and Developmental Biology, said: “We’ve uncovered a breakdown in how the brain consolidates memories, visible at the level of individual neurons.
“What’s striking is that replay events still occur, but they’ve lost their normal structure. It’s not that the brain stops trying to consolidate memories, the process itself has gone wrong.”
Professor Barry added that the findings may help researchers identify Alzheimer’s earlier or develop treatments that focus on restoring normal replay activity.
News
Blood test could spot pancreatic cancer earlier
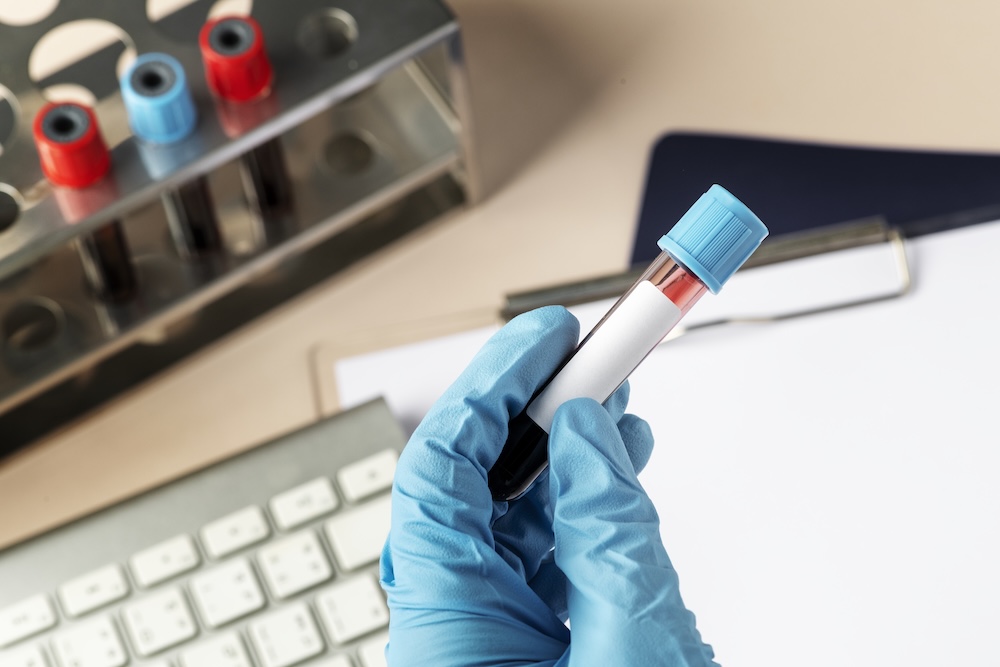
Scientists have developed a pancreatic cancer blood test that could detect disease earlier, potentially improving survival if validated in larger studies.
Around 10,500 people are diagnosed with the disease in the UK each year, but it is hard to treat and diagnose.
Because it is often found late, only 10 per cent live longer than five years after diagnosis, with more than half dying within three months of diagnosis.
Researchers from the University of Pennsylvania and the Mayo Clinic say the test could detect pancreatic ductal adenocarcinoma, the most common and one of the most aggressive forms of the disease, in its earliest stages, giving doctors time to treat it and increase patients’ chance of survival.
The team tested stored blood samples from people with pancreatic cancer and from people without it.
They examined two markers already used in medicine, CA19-9 and THBS2.
On their own these are not accurate enough for screening, as CA19-9 can be high in non-cancer conditions such as pancreatitis (inflammation of the pancreas) or bile duct problems, and some people do not produce it because of their genes. THBS2 is a protein linked with tissue changes around tumours.
The researchers discovered two additional proteins in the blood, ANPEP and PIGR, that were higher in people with early pancreatic cancer than in healthy volunteers.
When the team combined all four markers into one test, it correctly identified pancreatic cancer about 92 per cent of the time, at a 5 per cent false-positive rate.
For early-stage cancer, it picked up nearly 8 per cent of cases.
The researchers say the test could be used to screen people at higher risk, such as those with a family history, certain genetic risks, pancreatic cysts or long-term pancreatitis. It also distinguished cancer from non-cancerous conditions like pancreatitis, a key limitation of previous models.
Kenneth Zaret, the study’s lead investigator from the University of Pennsylvania’s Perelman School of Medicine, said: “By adding ANPEP and PIGR to the existing markers, we’ve significantly improved our ability to detect this cancer when it’s most treatable.
“Our retrospective study findings warrant further testing in larger populations, particularly in people before they show symptoms.
“Such ‘prediagnostic’ studies would help determine if the test could be used as a screening tool for people at high risk of developing the disease based on family history, genetic screening results or personal history of pancreatic cysts or pancreatitis.”
However, it could take years before the new blood test has completed the trials and regulatory steps needed for mainstream use.
At present, pancreatic cancer is incurable, with life expectancy just five years from initial diagnosis.
It kills because it aggressively invades nearby organs, blocks the bile and intestinal ducts, and spreads via the blood and lymphatic system to the liver, lungs and abdomen, eventually triggering organ failure.
The pancreas aids digestion and produces hormones, such as insulin and glucagon, which help convert sugar from food into energy. Pancreatic cancer can reduce the gland’s ability to make these hormones, which can lead to unstable blood sugar levels.
Common symptoms include jaundice (yellowing of the skin and eyes), loss of appetite, weight loss, fatigue, a high temperature, feeling or being sick, diarrhoea and constipation.
Research published last year suggested that more than half of patients diagnosed with the six least curable cancers, including lung, liver, brain, oesophageal, stomach and pancreatic, die within a year of diagnosis.
More than 90,000 people are diagnosed with one of these cancers in the UK every year, accounting for nearly half of all common cancer deaths, according to Cancer Research UK.
There are currently no early detection tests and about 80 per cent of people are not diagnosed until the cancer has spread, meaning life-saving treatment is no longer possible.
Last week, Spanish researchers revealed a treatment plan that made pancreatic cancer cells shrink in laboratory mice. However, this requires much more robust testing, meaning it could be years before similar treatments are offered to human patients.

 News4 weeks ago
News4 weeks agoInterview: GlycanAge launch first hospital-based tests

 News4 weeks ago
News4 weeks agoCaptioning glasses win AARP pitch at CES

 News3 weeks ago
News3 weeks agoShingles vaccine may slow biological ageing in older adults

 Technology4 weeks ago
Technology4 weeks agoCorsera Health raises US$80m to prevent heart disease

 News4 weeks ago
News4 weeks agoOlder male athletes may face increased risk of serious heart problems during exercise

 Wellness3 weeks ago
Wellness3 weeks agoThousands of men in England to be offered life-extending prostate cancer drug

 News3 weeks ago
News3 weeks agoNanoparticles target disease proteins in dementia

 News4 weeks ago
News4 weeks agoBillionaire Platt backs Engitix again with US$25m