Wellness
Many Americans have never had a hearing test, survey reveals

Forty-four percent of Americans aged 45 and up think about their hearing at least occasionally but 79 per cent say they have not had a hearing test in the last year.
The new study, released by Lexie Hearing on World Hearing Day (Friday 3 March), surveyed the hearing health behaviours of 1,000 Americans 45 and older to better understand how they think about and care for their hearing as they age.
Findings show that hearing is often overlooked, even among those who prioritise other areas of health. While three out of four people say their health is very important, more than a third have never had a hearing test yet undergo other routine preventative screenings
Among the 76 per cent of Americans who say their health is “very important” to them, only 18 per cent have had a hearing test in the past year, compared to 75 per cent who have visited a dentist, 75 per cent who have had an eye exam, and 45 per cent who have done both.
Nic Klopper, CEO of Lexie Hearing, which specialises in over-the-counter hearing aids for people with mild-to-moderate hearing loss, commented: “World Hearing Day represents a moment for everyone to evaluate their hearing and take the steps to treat hearing loss.
“With the FDA’s approval of over-the-counter hearing aids for mild to moderate hearing loss last year, it’s easier and more affordable than ever to take control of your hearing health so you can get back to enjoying the moments you love with family and friends.”
While hearing aids are now more accessible, two in five (40 per cent) people are still unsure where to get a hearing aid if they need it. More than half (54 per cent) say if they had a hearing issue or concern, they would contact their primary care physician first.
Last October, the FDA approved new regulations for the sale of over-the-counter hearing aids for mild to moderate hearing loss, removing a substantial barrier to hearing health and giving consumers the flexibility to purchase high-quality devices without a prescription in retail, pharmacy and online stores nationwide.
Hearing health can have an impact on overall health as untreated hearing loss can lead to isolation. Regular hearing aid use on the other hand has been associated with a lower prevalence of depression and has been shown to improve physical and cognitive health, including reducing the risk of dementia.
In recognition of World Hearing Day and to encourage more people to take action toward better hearing health, Lexie Hearing will be donating a portion of all March sales to its Lexie Cares initiative, to help provide better access to hearing worldwide.
“The first step in caring for your hearing is to take a hearing test,” said Klopper.
“Doing so will help you determine if you have hearing loss, how much and whether or not you could benefit from a hearing aid.”
News
Interview: Dr Matthew Bennett on building resilience and a pain-free healthspan
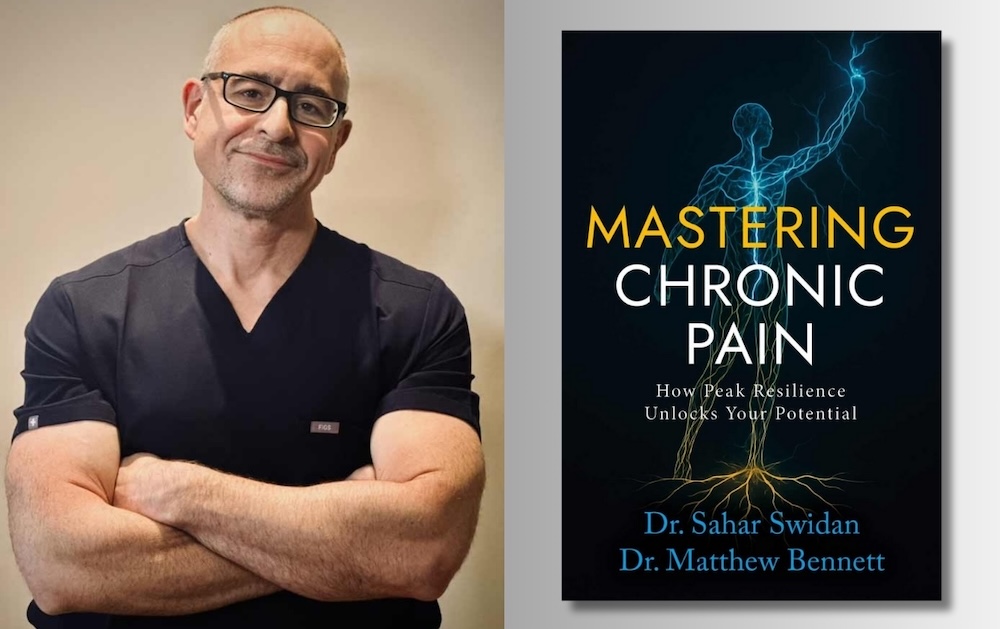
Harnessing the multi-dimensional capabilities of the human body is key to overcoming chronic pain and boosting longevity, say the authors of a new book.
While the primary focus of established health care systems is to target pain points through medication or surgery a more holistic approach is emerging, as US chronic pain doctor Matthew Bennett explains.
Published late last year by Dr Bennett and colleague Dr Sahar Swidan’s book, Mastering Chronic Pain: How Peak Resilience Unlocks Your Potential offers grounded insights into pain resolution.
Speaking to Agetech World from his New York base he said: “I’ve been treating patients in chronic pain for over 20 years.
“And, it becomes obvious that while some pain is very responsive to simple interventions, like a nerve block or a surgery, there’s a large number of people which that does not move the needle for.
“We used to look at it like, ‘Hey, the MRI shows this one spot that’s pushing on this one nerve. If we can take that spot off that nerve, everything’s going to be better’.
“And, that just doesn’t always play out that way. It’s become apparent that there are a lot of situations where the problem is more systemic.
“It’s really more of a metabolic problem, and pain is the expression of these system failures.”
‘Fight or flight’
The upstream drivers of acute pain can be numerous as Dr Bennett explains: “You can take as much pressure as you want off of nerves, but if your inflammatory system isn’t fixed, if the neurological system isn’t fixed, if your autonomic nervous system – meaning your fight-or-flight versus your rest-and-relaxation – isn’t balanced, if your gut biome is off, if your sleep is off – a lot of these problems aren’t going to improve.”
Key elements in developing a longevity-focused healthpsan – devoid of chronic pain and opioids – are simple, every day measures, focused on movement, sleep and breathing.
This includes developing the right muscles to create a ‘good deep core musculature’.
He continued: “An even bigger one is the way people breathe – the way they use their diaphragm.
“The diaphragm is a great big muscle that controls the deep core part of the spine. When the diaphragm’s not working correctly, the whole core musculature isn’t working right.
“You can’t get that stability in the lower spine, so other muscles jump in and try to do the work for you. That causes downstream problems.
“You need someone getting to that root cause,.. (and) we teach people how to do that, and they’ll have big breakthroughs.”
He continued: “Sleep is a big problem in people with chronic pain. There’s a lot of healing that occurs with deep sleep.
“Unfortunately, in a lot of pain states, sleep gets disrupted, and people can’t get into deep sleep, so the brain can’t clear itself of the byproducts of metabolism; that glymphatic system doesn’t work.
“Poor sleep also interferes with endocrine connectors; growth or sex hormones can be depleted. Obstructive sleep apnea can play a huge role. There’s just a big correlation between sleep disorders and chronic pain.”
Seeking calm
These key elements of Dr Bennett’s work – which has been described as ‘biopsychosocial’ – come concomitant with a keen focus on nervous systems, chronic inflammation and neuroplasticity.
Dr Bennett, co-founder of NoceViva, continued: “When we think about neurologics, one of the things that’s very far upstream of a lot of health is the balance between the fight-or-flight system and the rest-and-relaxation system – that autonomic nervous system.
“All of these things are ‘two-way streets’ with pain; meaning the pain can cause the dysfunction, and the dysfunction can cause the pain; it becomes this feedback cycle where things get entrenched in a bad loop.
“So, balancing that autonomic nervous system is a really helpful upstream fix to make. Simple things like breathwork. Some people do well with meditation.
“Some people do well with making sure they’re involved in hobbies. These are things that can help just calm that fight-or-flight system down.”
Nerves & neuroplasticity
Allowing ourselves to adjust to emerging health challenges is achievable in the right settings and with the right approach.
He continued: “The body’s nervous system has the ability to change. And it can change based on various inputs.
“The nervous system can become increasingly sensitised, or it can become de-sensitised. And so that’s one of the bigger things that we see in the chronic pain state, is this sensitisation that comes along with it.
“This neuroplasticity can make the nerves in the extremities more sensitive.
“It can also make the nerves in the central nervous system more sensitive – so nerves in the spinal cord, or even nerves in the brain can become hyper-sensitised – so they’re triggering more of a pain response in the person.
“But the same thing that can cause the system to go in what we would consider a bad direction, where it gets more sensitive, the neuroplasticity can actually become undone, and you can make the nerves less sensitive.”
AI to boost lifespan?
Looking ahead Dr Bennett foresees a future where a deeper understanding of the functional pathways of pain, combined with AI, stem cell therapies and regenerative biologics will all speak to a future of greater longevity for mankind.
“I think the more attentive we are to the root cause, the more attentive we are to functional pathways – when we start thinking about how the system really works? And we get out of just an algorithmic approach to things.
“We still have quite a ways to go. I think we are making progress. There was a time where we would not be thinking about any of this.
“I think everyone’s excited about what AI will bring. And are we going to be able to make some big steps? I think we’re able to intervene on a genetic level at this point.
“Will we be able to do it well enough to change lifespan? I would guess, yes, but by how much? I don’t know!”
News
Study reveals link between cheese and dementia

A 25-year Swedish study links higher cheese intake to lower Alzheimer’s risk in people without known genetic risk, with cream also tied to lower dementia risk.
However, researchers emphasise that the results should be interpreted with caution.
The study tracked 27,670 people over 25 years.
During that time, 3,208 participants were diagnosed with dementia.
Among individuals without a known genetic risk for Alzheimer’s disease, those who consumed more than 50 grams of full-fat cheese per day showed a 13 to 17 per cent lower risk of developing Alzheimer’s.
This association did not appear in participants who carried genetic risk factors for the disease.
People who consumed more than 20 grams of full-fat cream per day also showed a lower risk of dementia overall, ranging from 16 to 24 per cent.
No meaningful links were found for low-fat or high-fat milk, fermented or non-fermented milk, or low-fat cream.
The results stand out because public health guidance has long encouraged people to choose low-fat dairy to protect heart health.
This connection matters because cardiovascular disease (conditions affecting the heart and blood vessels) and dementia share many underlying risk factors, including high blood pressure, diabetes and obesity.
When evidence from previous studies is combined, analyses suggest that cheese consumption may also be linked to a lower risk of heart disease, and that full-fat dairy does not necessarily increase cardiovascular risk.
Several other studies have explored whether similar patterns apply to brain health, but the results are mixed.
Evidence overall suggests that studies conducted in Asian populations are more likely to report benefits of dairy consumption for cognitive health (the ability to think, remember and reason), while many European studies do not.
One possible explanation is that average dairy intake tends to be much lower in Asian countries, meaning modest consumption may have different effects than higher intakes.
For example, one Japanese study reported a reduced dementia risk among people who ate cheese, but overall consumption levels were very low and the research was sponsored by a cheese producer.
In contrast, another Japanese study funded by government grants found no protective effect of cheese.
Some long-term European studies have also reported benefits.
In a Finnish study of 2,497 middle-aged men followed for 22 years, cheese was the only food associated with a lower dementia risk, reduced by 28 per cent.
Other dietary factors also appear to matter.
Higher consumption of milk and processed red meat was associated with worse performance on cognitive tests, while fish intake was linked to better results.
A large study in the UK that followed nearly 250,000 people found lower dementia risk among those who ate fish two to four times a week, fruit daily and cheese once a week.
However, these studies have important limitations.
What people eat is usually self-reported, and changes in memory can affect both eating habits and how accurately people remember what they have eaten. To deal with this, the Swedish researchers took two extra steps.
First, they excluded anyone who already had dementia when the study began.
Then they repeated the same calculations after removing people who went on to develop dementia within the first ten years of the study.
This did not mean starting the study again or recruiting new participants. It simply meant re-checking the results using a smaller group of people who remained dementia-free for longer.
The reason for doing this is that the early stages of dementia can subtly change behaviour long before diagnosis.
People may eat differently, lose appetite or struggle to recall their usual diet. By focusing on participants who stayed cognitively healthy for many years, the researchers reduced the chance that these early changes were influencing the results.
Another important question is whether substitution played a role.
Some of the apparent benefits may reflect replacing red or processed meat with cheese or cream, rather than an effect of dairy itself.
Supporting this idea, the Swedish study found no association between full-fat dairy and dementia risk among participants whose diets remained stable over five years.
Most importantly, foods should not be considered in isolation.
Dietary patterns matter more than individual ingredients. Diets such as the Mediterranean diet, which is consistently associated with lower risks of both dementia and heart disease, include cheese alongside vegetables, fish, whole grains and fruit.
In the Swedish study, people who consumed more full-fat cheese and cream were also more educated, less likely to be overweight and had lower rates of conditions linked to dementia, including heart disease, stroke, high blood pressure and diabetes.
All of these factors independently reduce dementia risk.
This suggests that higher cheese intake tended to occur within healthier overall lifestyles, rather than alongside excess calorie consumption or poor metabolic health.
Overall, the evidence does not support the idea that full-fat dairy causes dementia, nor that fermented milk products reliably protect against it.
Full-fat cheese contains several nutrients relevant to brain health, including fat-soluble vitamins A, D and K2, as well as vitamin B12, folate, iodine, zinc and selenium.
These nutrients play roles in neurological function and may help support cognitive health.
That said, the data do not justify eating large amounts of cheese or cream as protective foods against dementia or heart disease.
The most consistent message remains that balanced diets, moderation and overall lifestyle matter far more than any single item on the cheese board.
News
New obesity and diabetes drug set for Boots clinical trial

 News4 weeks ago
News4 weeks agoInterview: GlycanAge launch first hospital-based tests

 Wellness3 weeks ago
Wellness3 weeks agoShingles vaccine may slow biological ageing in older adults

 News4 weeks ago
News4 weeks agoOlder male athletes may face increased risk of serious heart problems during exercise

 News3 weeks ago
News3 weeks agoThousands of men in England to be offered life-extending prostate cancer drug

 News3 weeks ago
News3 weeks agoNanoparticles target disease proteins in dementia

 News3 weeks ago
News3 weeks agoL-Nutra raises US$36.5m in series D funding

 News4 weeks ago
News4 weeks agoBlood sugar spike after meals may increase Alzheimer’s risk

 Insights4 weeks ago
Insights4 weeks agoStudy reveals why memory declines with age